
Understanding Gestational Diabetes: Insights from Dr Shruthi Kalagara

Author: Dr. Shruthi Kalagara, Obstetrician - Gynecologist
Understanding Gestational Diabetes: Insights from Dr Shruthi Kalagara
Gestational diabetes mellitus (GDM) is one of the most common medical complication in pregnancy, affecting around 1 in 6 births. As a high-risk pregnancy obstetrician, I believe it’s essential to provide accurate, supportive, and comprehensive information to help expectant mothers navigate this condition with confidence and care.
What is Gestational Diabetes?
Gestational diabetes is a type of diabetes that develops exclusively during pregnancy and typically resolves after delivery. It affects how your body processes glucose, leading to elevated blood sugar levels that can impact both the mother and baby if not managed appropriately.
Causes and Risk Factors
Hormonal changes during pregnancy play a significant role. The placenta produces hormones that can make your cells less responsive to insulin. When your pancreas can’t produce enough insulin to compensate, blood sugar levels rise, leading to GDM.
Certain factors can increase the risk of developing GDM, including:
- Age: Women over the age of 35 are at higher risk.
- Family or Personal History: A family history of diabetes or a previous pregnancy with GDM, previous big baby >/= 4.5kg birth weight raises the likelihood.
- Obesity: Being overweight before pregnancy is a significant risk factor.
- Ethnicity: Women of certain ethnic backgrounds, including South Asian, Indian, African American, and Hispanic, have a higher risk.
- Polycystic Ovary Syndrome (PCOS): This condition can contribute to insulin resistance and increase the risk.
- Inter-pregnancy weight gain: Increases recurrence risk.
Potential Impacts on Mother and Baby
Untreated or poorly managed gestational diabetes can lead to complications such as:
Short term and long term implications
- For the Baby:
- Macrosomia: Babies born larger than average, which may complicate delivery and increase the likelihood of cesarean birth.
- Neonatal Hypoglycemia: Low blood sugar in the baby shortly after birth.
- Neonatal Hyperbilirubinemia: Jaundice in the baby shortly after birth.
- Respiratory distress in newborn.
- Increased Risk of Obesity and Type 2 Diabetes: Children may be at a higher risk later in life.
- For the Mother:
- High Blood Pressure and Preeclampsia: GDM can elevate the risk of developing preeclampsia, a condition that can be dangerous if not managed.
- Urinary tract infection/ vaginal infections
- Obstetric intervention: instrumental deliveries, cesarean deliveries, postpartum hemorrhage.
- Future Diabetes: Women who develop GDM have a higher risk of developing type 2 diabetes in the future.
Diagnosing Gestational Diabetes
Universal screening for GDM is typically done between 24 to 28 weeks of pregnancy using an oral glucose tolerance test (OGTT) - 75g. For women with higher risk factors, testing may be recommended earlier in pregnancy.
Managing Gestational Diabetes
The good news is that gestational diabetes can be managed effectively with the right approach:
- Diet and Nutrition: A balanced diet rich in fiber, lean proteins, and complex carbohydrates helps regulate blood sugar levels. Consulting a registered dietitian can be beneficial.
- Exercise: Regular, moderate exercise helps improve the body’s insulin sensitivity.
- Blood Sugar Monitoring: Keeping track of your blood sugar levels is crucial to ensure they remain within the target range.
- Medication: If lifestyle modifications are not enough, medications or insulin therapy may be needed.
Support and Guidance:
Dealing with a high-risk pregnancy, such as one complicated by gestational diabetes, can be overwhelming. However, with proper care, monitoring, and guidance, most women with GDM go on to have healthy pregnancies and babies. It’s vital to work closely with your healthcare team, including an obstetrician specialized in high-risk pregnancies, to create a personalized care plan.
Postpartum Care
Gestational diabetes typically resolves after birth, but it’s essential to maintain regular follow-up visits and screenings. Women with GDM should have a glucose tolerance test six weeks postpartum and continue to monitor their health in subsequent years.
Final Thoughts
Gestational diabetes is a condition that requires attention, but it doesn’t have to define your pregnancy experience. With awareness, proactive management, and support, you can enjoy a healthy and positive journey to motherhood.
For personalized care and expert advice, don’t hesitate to reach out to your obstetrician. Your health and the well-being of your baby are always the top priority.
Related Blogs

Understanding Different Types of Vaginal Birth Delivery
Read More
How to Treat and Prevent Brown Discharge
Read More
Endometriosis Understanding, Diagnosing, and Managing the Condition
Read More
Emotional Support During IVF Treatment
Read More
Urinary Tract Infection (UTI) in Pregnancy
Read More
Early Pregnancy Care for New Pregnant Women: Expert Advice | Motherhood Hospitals
Read More
Body Positivity Tips Post C Section (Cesarean Delivery)
Read More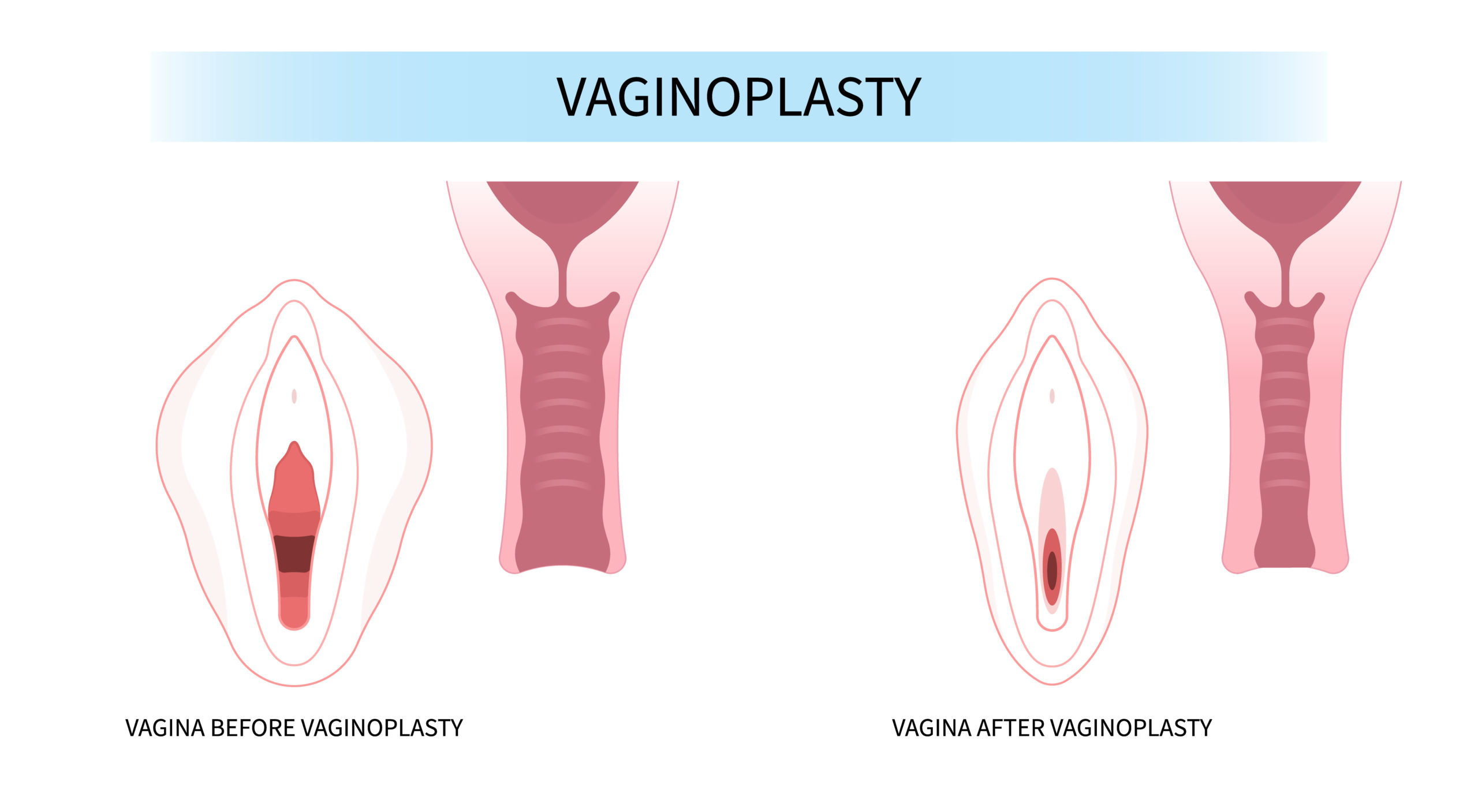
Vaginoplasty: Procedure, Cost, Risks & Benefits, Recovery
Read More
The Digital Dilemma: Exploring the Medical Implications of Technology on Child Development
Read More
How To Relieve Menstrual Cramps? - 8 Simple Tips
Read MoreRequest A Call Back
Leave a Comment:
View Comments
Previous
Next
HELLO,
Stay update don our latest packages, offer, news, new launches, and more. Enter your email to subscribe to our news letter


 Toll Free Number
Toll Free Number








No comment yet, add your voice below!