The silent threat of female genital TB in LMICs
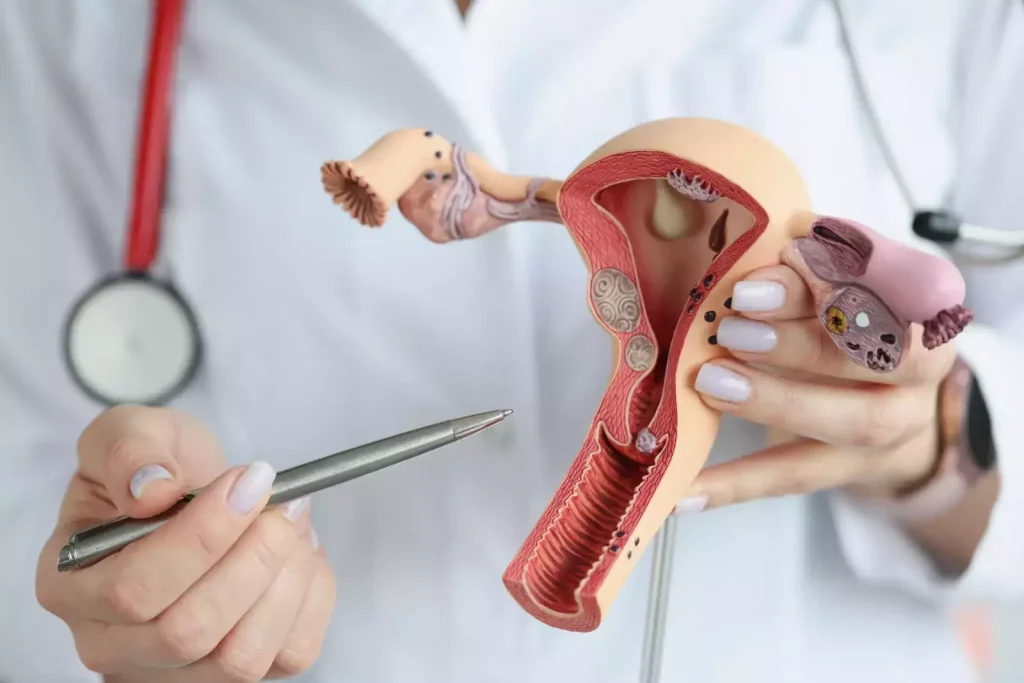
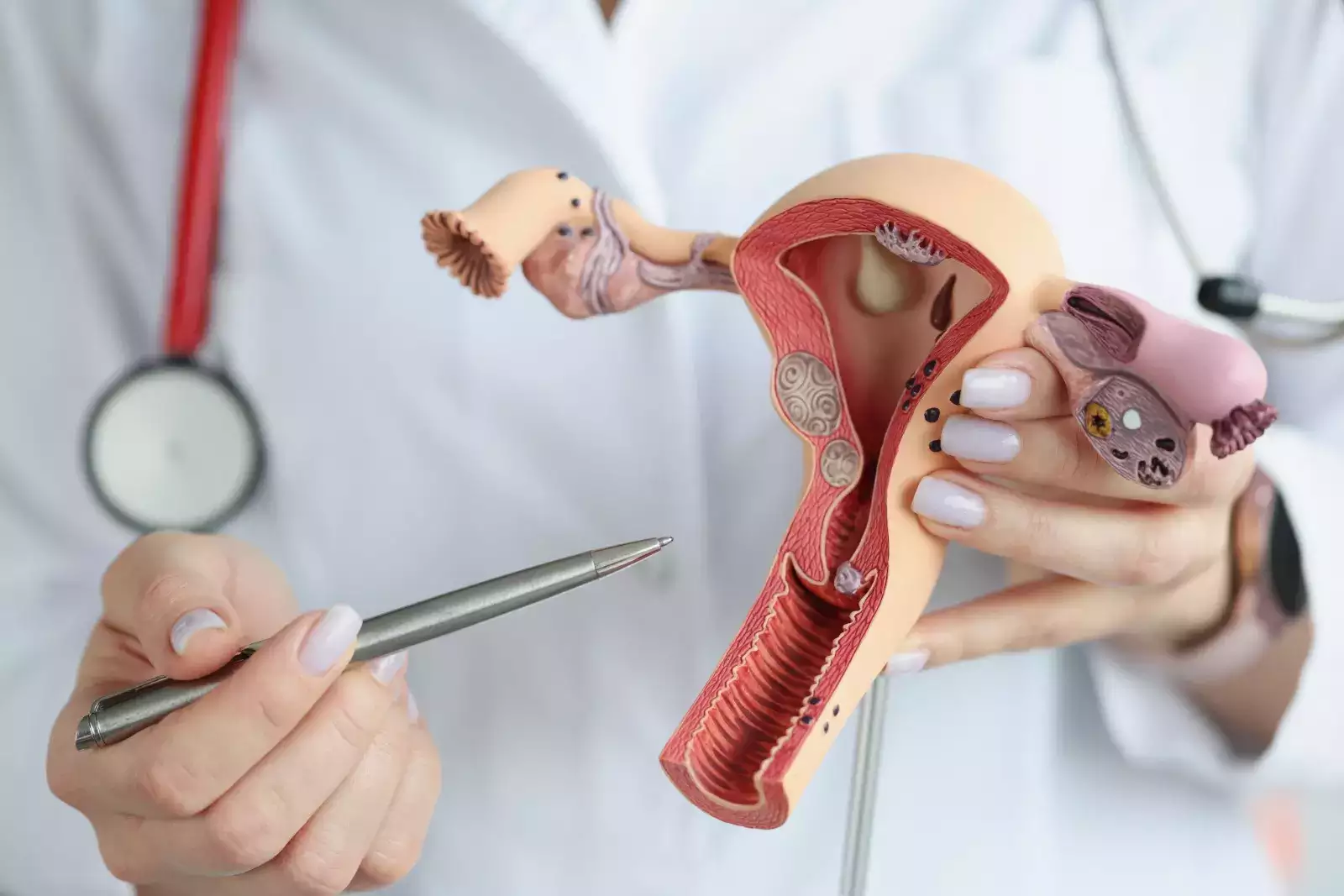
New Delhi: Women across age groups are mostly not aware of female genital TB (FGTB), as there are no symptoms; it is a silent disease sparing no age group but the majority of patients that are affected are of reproductive age. As per doctors, FGTB causes significant morbidity also a major reason for infertility. Experts inform that it is still an underestimated disease, which needs awareness and prompt attention and a high degree of evaluation by doctors for correct diagnosis and treatment. On the occasion of World TB Day, ETHealthworld spoke with doyens of fertility with diverse experience to gain a clear understanding of not only the severity of FGTB but also how it is frequently diagnosed at later stages, when the disease’s scope has widened and has the potential to have a devastating impact on women’s reproductive health. A study published in the Indian Journal of Tuberculosis suggests 25 per cent of the women who suffer from pulmonary TB in India also have silent genital tuberculosis. Mycobacterium tuberculosis (occasionally Mycobacterium bovis and/or atypical mycobacteria) is the primary causative agent of FGTB. It typically develops as a result of TB of the lungs or other organs and spreads by lymphatic, haematogenous, or direct dissemination from abdominal TB. Around 90 per cent of women with FGTB experience fallopian tube damage.


 Toll Free Number
Toll Free Number