India has been making great headway in the eradication of diseases like Polio & Small Pox but this is just the tip of the iceberg. Certain conditions like Anaemia do not get the attention they deserve. Characterized by subtle symptoms, diseases of this nature can go untreated for a long period leading to serious complications or occasionally even death. Women may be totally unaware that they are suffering from such conditions.
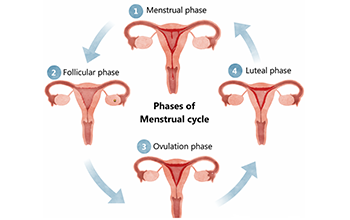
Anaemia in varying degrees is widely prevalent amongst Indian women. Global Nutrition Report 2017 states that about 51% of women of reproductive age in India suffer from anaemia. It is predominantly due to nutritional deficiency. Women also have to cope with blood loss during their monthly periods which can further reduce their haemoglobin levels. It is prevalent across all socioeconomic strata and is a condition that can be easily diagnosed and treated.
Anaemia characterized by low blood hemoglobin levels increases the risk of infection, preterm delivery, and suboptimal fetal growth. In infancy and early childhood, Anaemia can cause recurrent illness, failure to thrive, poor performance at school and failure to participate in physical training and games at school. Analysis by a think tank, IndiaSpend, states that anaemia has remained the leading cause of disability across the ages in India for the past 10 years. Anaemia can be easily diagnosed by a simple blood test called Complete Blood Count.
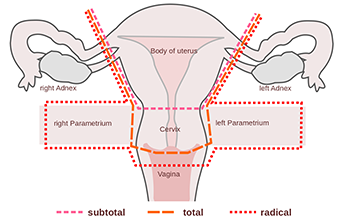
Cervical cancer is a leading cause of death from cancer amongst Indian women. It runs parallel to breast cancer in incidence. A study on cervical cancer by ASSOCHAM-National Institute of Cancer Prevention and Research (NICPR) reveals India alone accounts for one-fourth of the total cervical cancer burden globally. Almost 17% of cancer-related fatalities in women between the age of 30-69 can be attributed to cervical cancer. Majority of cervical cancers in India even today are diagnosed at a late stage. There is, however, an opportunity to detect precancerous changes of the cervix at least 15 to 20 years ahead by a simple test known as the Pap Smear. This test, although widely available to the affluent classes, is not easily accessible to the lower social strata. Cervical Cancer, however, unfortunately, is more prevalent in this lesser privileged section of our society.
Simple tests such as Pap Smears & Complete Blood Count (CBC) can go a long way in not only saving the lives of many Indian women but also improving their quality of life. Due to the rapid changes in lifestyles as well as lack of awareness of such diseases, our mothers, sisters and daughters fall victim to these ‘unnoticed killers’. What is even more alarming is that due to the high cost associated with such tests many women from the underprivileged sections of our society may not have access to such lifesaving screening tests.
In an effort to create awareness amongst our women and in order to provide women from the underprivileged section of our society an opportunity to avail these tests Motherhood Women and Children hospital conducted a free medical camp for women in partnership with the Thuluva Vellala Association. Basic history, examination, blood counts, blood sugars, ECG and BP and Pap-smears test were performed and referrals to specialists were made if required. The camp was attended by more than 150 men and women. A significant number of women were benefited by the special services offered at this camp.


 Toll Free Number
Toll Free Number