Consultant – Obstetrician & Gynaecologist at Motherhood Hospitals, Alwarpet
It’s good to know your due date when you are pregnant. And this is much easier if you have a pregnancy calculator. Every woman can use the pregnancy calculator to track her pregnancy schedule and due date.
With pregnancy comes family planning and sometimes it may become overwhelming. The excitement is real, but so is the work and the stress. With a child on the way, family planning becomes more significant.
With the help of a pregnancy week calculator, you, the ‘Mother-to-be’ can keep track of your pregnancy schedule based on the date of your last period, ultrasound, and conception.
Pregnancy Week Calculator
The Pregnancy Week Calculator helps women confirm their pregnancy and track the week of pregnancy they are currently in. Based on that, the woman can plan her visit to the doctor/ check up.

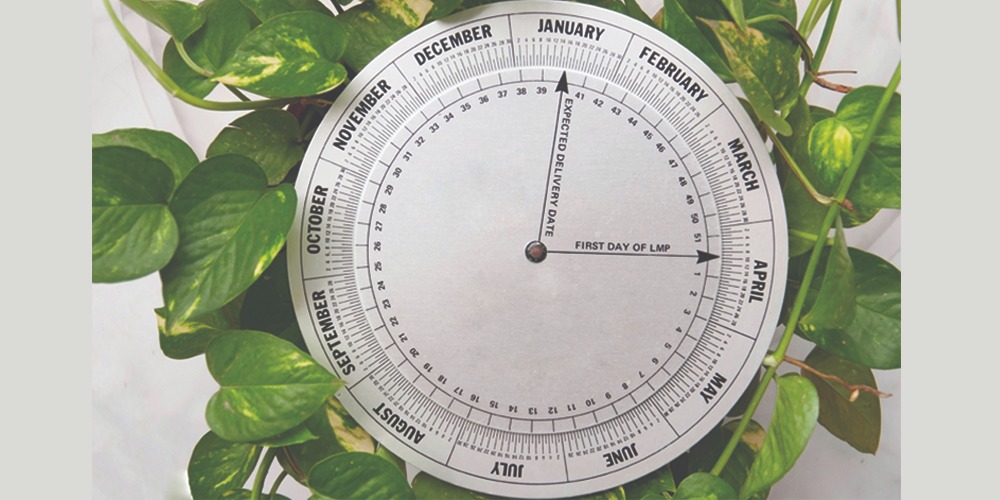
The Pregnancy Week Calculator by due date helps women to prepare for the delivery date. However, it is essential to note that not every baby is born on the exact estimated due date. Only 4% of all babies are born on the estimated due date. Some are born within weeks of the due date. Usually, every healthy pregnancy lasts up to 37 to 42 weeks. The usual way to estimate the due date is to count 280 days (40 weeks) from the first day of the woman’s LMP or Last Menstrual Period.
Those who might have forgotten their LMP or cannot seem to figure out the time of their LMP can go or opt for an ultrasound. This can confirm if the woman is actually pregnant and can also determine her the date of delivery.
Once your pregnancy is confirmed, you will notice a lot of changes in your body. Based on that, you and your partner can start planning accordingly. This is where it will get all the more exciting and stressful, marking the beginning of the wonderful journey towards parenthood.
Pregnancy Calculator Week by Week
Using the Pregnancy Calculator Week by Week you can share your motherhood experience with your partner. In the 9th / 10th week of your pregnancy, you can hear your baby’s heartbeat for the first time. It’s one of the most beautiful moments you will experience during the start of your pregnancy.
Between the 18th and 22nd week of your pregnancy, you might start feeling your baby’s movement inside you. You can feel fetal movement earlier or sometimes later. With the help of the Pregnancy Calculator you can determine if you are due for anomaly scan.
Another essential aspect of pregnancy is that the due date may vary. It is not always necessary that the baby will be born on the assigned due date as mentioned earlier. Don’t let this stress you out. Stress is neither good for you, nor for the baby. However, with your partner and Pregnancy Calculator, it will become easier for you to prepare for the event.
It is always good to have plans made ahead of the due date. With the data provided by the Pregnancy Week Calculator, you can prepare well for the D Day. Always remember to reach out to your doctor in case you are unsure of something. Keep in mind that you and your partner need to be calm and plan wisely for the baby. But don’t forget to enjoy the experience of bringing a healthy child into the world. You can make a birth plan and discuss with your doctor.
At Motherhood Hospitals, we have a team of experienced super specialists backed by the latest in infrastructure and facilities. We have the best experts in Alwarpet, Chennai capable of handling complex deliveries, gynaecological and other surgeries including a range of laparoscopic procedures.
Do take an appointment with the best Gynaecology hospital in Alwarpet, Chennai at a centre closest to you. Meet with our doctors who will carry out the required investigations, diagnose the issue and recommend the most appropriate treatment, enabling you to lead an active life.
If you wish to get in touch with Dr.Kavya Krishna kumar, please book your appointment here.


 Toll Free Number
Toll Free Number