Laparoscopy plays a very important role in the management of subfertility. Its suggested for women where after the basic investigation like hysterosalpingogram for tube assessment, ultrasound for assessment of uterus and ovary, and hormone analysis for the female partner and semen analysis in a male partner have not yielded any reason for subfertility or when on ultrasound in female partner has shown certain abnormality .
Laparoscopy is a very simple procedure. In subfertility usually it a day care procedure.it is done under anaesthesia but hysteroscopy can be done without anaesthesia which we call it as office hysteroscopy. Like women is admitted in the morning and discharged by evening, as it being diagnostic in nature most of the time. Even if we have do some corrective procedure like adhesiolysis, drilling, cystectomy, tubal cannulation, polypectomy or septal resection
Usually in a diagnostic lap with create 2 small incision of 5mm on the abdomen through which lap instruments are passed through and the procedure completed. If we need to do some operative procedure like cystectomy or adhesiolysis we create one more incision. As the cut are very small the problems associated with surgery is very minimal. Patient generally do not complain of pain and usually can go back to normal routine work in a days?? time.
Although there are many scientific methods to treat infertility such as in vitro fertilization (IVF) assisted reproductive technologies (ART), laparoscopy is inevitable in conditions where the reasons for infertility remain unknown.
When is diagnostic laparoscopy for infertility recommended?
After the initial work up of the couple if we find that there??s no obvious reason for subfertility then we recommend further investigation with diagnostic hystero- laparoscopy. And also when there are certain indications like
- In case of an previous pelvic surgery
- In case of suspected mild to moderate endometriosis.
- In case of suspected pelvic inflammatory disease or tuberculosis.
- In case of severe pain and cramps during menstrual cycles.
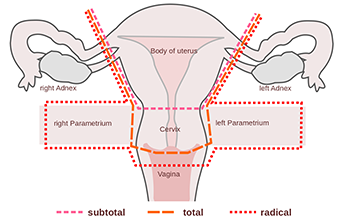
When is laparoscopic surgery recommended?
Is indicated when on initial investigation reveals certain correctable causes of subfertility.
- In case of polycystic ovarian syndrome
- In case of an endometrial deposits
- If the fallopian tubes are blocked
- If Hydrosalpinx is suspected
- If ovarian cysts block fallopian tubes
Benefits of Laparoscopy:
- Helps in having a comprehensive and detailed look inside the abdominal region
- Helps in getting rid of pelvic pain
- Helps in removing scar tissues, fibroids, and endometrial deposits


 Toll Free Number
Toll Free Number