Pregnancy can lead to dental problems including gum disease and an increased risk of tooth decay.
During pregnancy increased hormonal changes can affect the body’s response to the plaque on your
Teeth. However, the demands of pregnancy can lead to particular dental problems in some women,
With proper hygiene at home and professional help from your dentist, your teeth should remain
healthy throughout pregnancy.
Dental disease can affect a developing baby
Research has found a link between gum disease in pregnant women and premature birth with low
Birth weight. Babies who are born prematurely may be at risk of a range of health conditions including
Cerebral palsy and problems with eyesight and hearing.
Estimates suggest that up to 18 out of every 100 premature births may be triggered by periodontal
disease, which is a chronic infection of the gums. Appropriate dental treatment for the expectant
mother may reduce the risk of premature birth.
Causes of dental health problems:
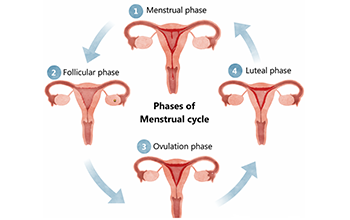
Gum problems The hormones associated with pregnancy can make women susceptible to gum
problems like gingivitis (gum inflammation), more likely to occur from the first trimester with
symptoms including swelling of the gums and bleeding particularly during brushing and when
flossing between teeth.
Undiagnosed or untreated periodontal disease, pregnancy may worsen this infection and can
lead to tooth loss.
Pregnancy epulis, a localized enlargement of the gum, which can bleed easily.
During pregnancy, the gum problems that occur are not due to increased plaque, but a worse
response to plaque as a result of increased hormone levels.
Tooth Decay- Some women experience unusual food cravings while they are pregnant and a
regular desire for sugary snacks may increase the risk of tooth decay.
Morning sickness- Pregnancy hormones can cause gastric reflux (regurgitating food or drink) or
the vomiting associated with morning sickness that can coat the teeth with strong stomach
acids. Repeated reflux and vomiting can damage tooth enamel and increase the risk of decay.
Dental treatment and Pregnancy: Safety Factor
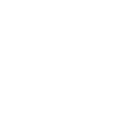
The safest time to undergo dental treatment is the 2 and trimester of pregnancy. Preventive
scaling or professional cleaning of the gums and teeth, cavity fillings and annual dental check-
ups during pregnancy are not only safe but are recommended. Elective treatments such as teeth
whitening and other cosmetic procedures should be postponed until after birth. However,
sometimes emergency dental procedures like tooth extraction or a root canal treatment can be
performed under precaution and following strict protocols.
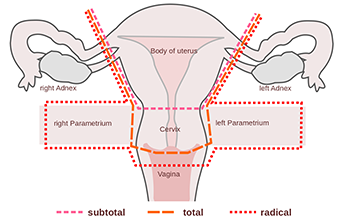
Medications: Anesthesia is an integral part of dental procedures if needed the amount of
anesthesia to be administered should be as little as possible, but enough to make the patient
comfortable, at times additional anesthesia may be required. According American Dental
Association controlled administration of local anesthesia does not cause any significant harm to
the developing baby or the mother. Certain group of antibiotics and analgesics can safely be
prescribed throughout the 9 month pregnancy period.
X-rays: Routine x-rays typically taken during annual check-ups can usually be postponed until
birth. X-rays are necessary to perform many dental procedures especially emergencies. According
to American College of Radiology, no single x-ray has a radiation dose significant enough to cause
adverse effects in a developing embryo or fetus with appropriate shielding.
Treatment Planning during Pregnancy:
1. All pre-existing dental issues need to be sorted out before planning for a child, it is
recommended.
2. If already pregnant with pre-existing dental issues, it is advised to inform the dentist about
the pregnancy, the stage of pregnancy and the due date for the delivery. This information is
very important for the dentist to plan and execute the best possible oral care.
Home oral Care:
1. Brush your teeth with fluoridated toothpaste twice daily.
2. Floss your teeth regularly and rinse your mouth with an alcohol-free mouthwash.
3. Replace the toothbrush every month and use a soft bristle toothbrush.


 Toll Free Number
Toll Free Number