NICU LIVE BY MOTHERHOOD
An Innovative Virtual Neonatal Intensive Care Solution from Motherhood Hospitals
The Vision
To make Quality intensive care facilities available to all critically ill infants, in urban and remote areas.
India records around2.3 million neonatal deaths yearly due to a lack of quality health services.
Motherhood, India’s leading network of women and children’s hospitals, has launched the first of its kind NICU – Live neonatal services, a state-of-the-art Intensive Care Management solution available remotely.
NICU aims to make world-class neonatal care accessible to new-borns, wherever they may be. The solution offers simple-to-use yet effective innovative technology that enables high-quality clinical expertise to deliver tailor-made patient-centric solutions.
NICU Live is conceived to upgrade your NICU by improving capacity utilization, and digitization, while also providing continuous advanced-level training for nurses.
“CONNECTING CRITICAL CARE, SAVING LIVES!”
How NICU LIVE Works the Magic?
NICU Live’s innovative remote monitoring and assistance program uses technology to save a newborn life, time, and money. Motherhood NICU Live’s remote NICU solutions attend to critically ill newborns, remotely.
Running on a simple hub-and-spoke model, NICU Live is designed to benefit numerous families, where accessibility to neo-natal healthcare expertise and 24×7 monitoring is out of bounds. It aims to augment the productivity and capacity of doctors and nurses in urban as well as remote centers seeking to upgrade their facilities. It is an effort to give babies a new lease of life by delivering advanced neonatal intensive care, which it was a challenge earlier.
NICU Live is powered by, a cutting-edge digital platform that facilitates collaboration, active clinical operations, and outcomes analysis. It facilitates role-based workflows, actionable alerts, and machine-learning tools.
It provides a remote connection to Motherhood’s specialized team of Neonatologists, skilled nurses, and medical experts with the local healthcare center. This connection offers neonatal emergency care, allowing them to monitor urgent medical conditions around-the-clock. The NICU solution enhances the productivity of the doctors and nurses to attend to critical babies and offer advanced diagnosis and treatment plans.
The solution will help to upgrade the existing remote NICU to an advanced level by:
- Improving capacity utilization
- Enabling efficiency through digitization
- Providing continuous advanced-level training for nurses
NICU Live ensures that distance and time never stand as a barrier to saving young lives – and technology truly supports this vision!
NICU Delivers:
NICU Live’s remote healthcare center will be connected nodally to the central care center (managed by Motherhood Hospital’s in-house expert team) using state-of-the-art tools.
The NICU Live solution delivers:
- A NICU Live platform that makes remote neo-natal monitoring available, with access to a multidisciplinary expert team.
- 24*7 management, nursing, and consultation of patients by highly-experienced and trained clinicians from Motherhood.
- Live monitoring of the vitals and conditions of the baby.
- Enhanced productivity and quality of life for caregivers.
- Shorter hospital stays and better resource utilization, for higher patient turnaround.
- Capability to handle more severe and critical cases.
- Lower transfers and increased footfall.
- Efficient clinical operations, potential risks, and analysis, thereby maximizing focus on the remote team’s patient care services.
- Ensures role-based workflows and actionable alerts through machine learning tools.
- Improved clinical outcomes.
With the power of Digitization, NICU Live offers:
- 24×7 availability.
- Remote access allows healthcare experts to offer their services to patients without geographical boundaries.
- Digital database capabilities- delivering paperless documentation and records.
- Ability to derive Insightful analytics.
- Central data repository of all lab reports, x-rays, and prescriptions.
- Proactive monitoring tools onsite, leading to Improved healthcare outcomes.
- Automated vital parameters entry, facilitates medication administration seamlessly, and the availability of lab and radiology results without delay.
- Quick and easy collaboration between the bedside doctors and specialists from the remote center through notifications, secure chats, video conferencing, and high-definition video feeds.
- Medical intelligence is the perfect assistant to auto-complete notes, take dictations, and keep the ICU running and patients safe.
NICU Product Solution
NICU LIVE: REDEFINING NEONATAL CARE WITH THE POWER OF TECHNOLOGY!
24*7 advanced remote patient management made possible with NICU Live by Motherhood.
The Story of How NICU Saves Lives with Technology
NICU Live uses the following technologies to implement its Neonatal Care Solutions:
A Web-based and Mobile Application
NICU Live’s digital platform makes maintaining medical records and data entry seamless and convenient. All medication charts, vitals, lab results, and doctors’ orders are uploaded on one common platform – creating a link of timely communication between Motherhood Nodal and the remote centers possible.
The RADAR: Productivity tools that make all this possible:
- An ML-powered note-writing assistant that reduces documentation time by 40%.
- An Automated document transcription that integrates and digitizes paper data.
- An efficient computer vision tool that increases nursing efficiency by 30%.
- Voice-to-text dictation tool that allows for documentation and clear understanding of instructions and prescriptions to be issued.
PTZ Cameras
The high-definition PTZ cameras are installed at all remote centers for a 24*7 live feed. This camera captures 360-degree movement for in-depth case analysis, allowing the remotely-placed nurses and caregivers to zoom in to see babies and identify even their breathing patterns.
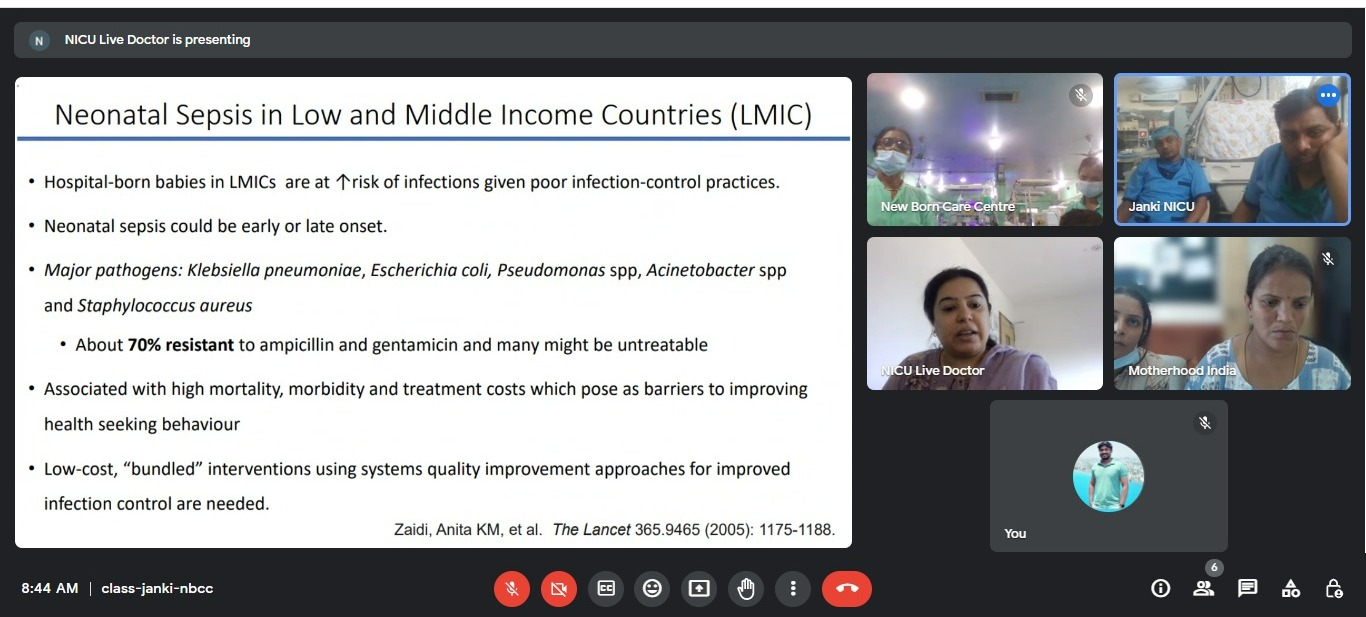
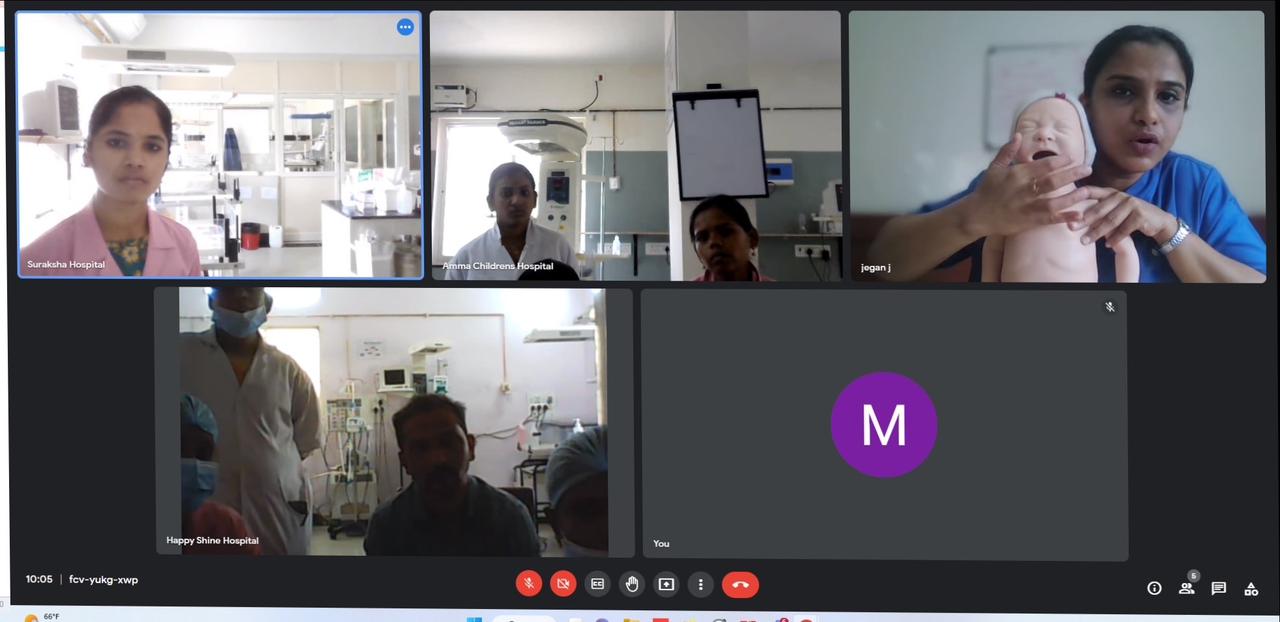
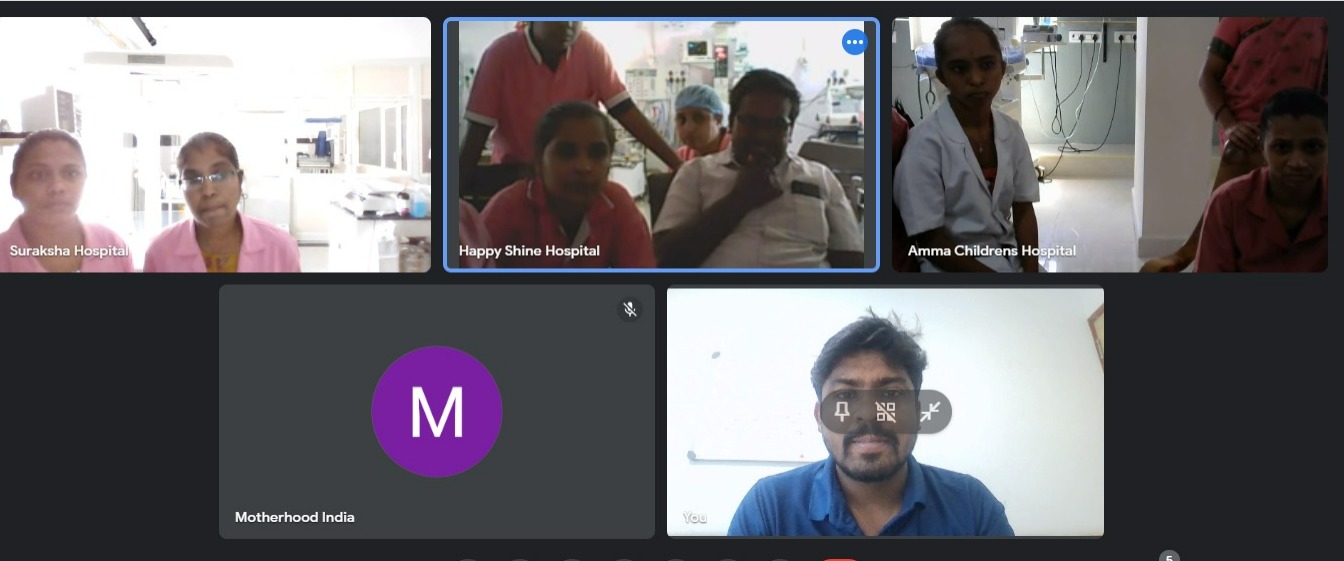
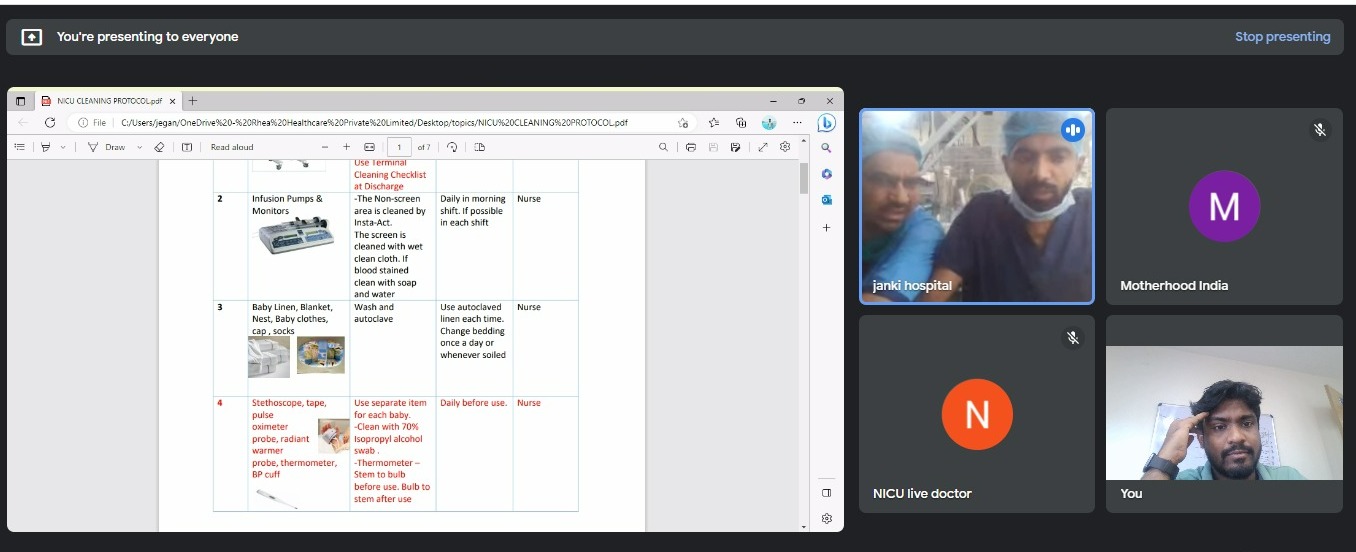
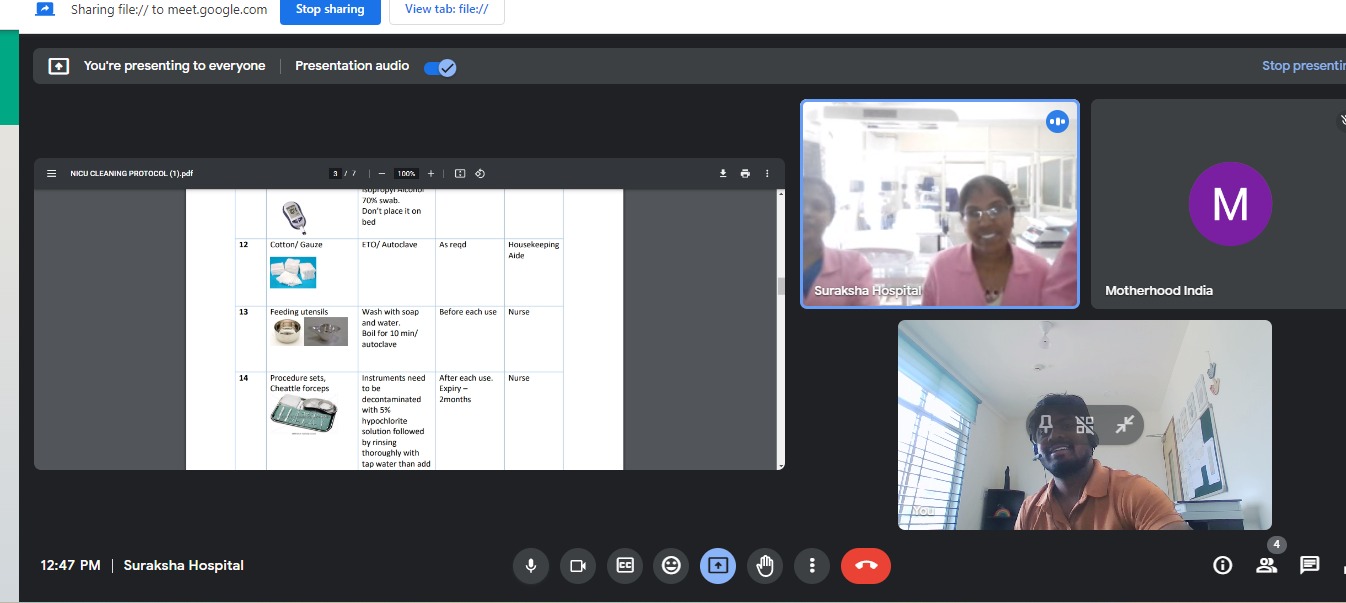
Communication Enablement
24*7 communication enablement by NICU Live arranging virtual calls between Hub Nurse, Hub Doctor, and NICU unit, offering instant solutions and treatment plans. The solution also offers a chat option for real-time data sharing. There is also a WhatsApp integration for operational coordination.
Also, NICU Live ensures the security and compliance of all medical data and patient records. By implementing the best industry practices, NICU Live works towards improving the quality of neonatal care.
Issues faced by neonatal ICUs:
- 24 * 7 availability of quality clinicians
- Lack of expertise at the nursing level
- Severe cases getting transferred
- Management of records
- Wastage of time struggling to find advanced solutions Ensuring continuous learning for nurses
NICU Live tackles this by:
- Real-time 24/7/365 management of patients by an expert team of clinicians
- Availability of highly skilled NNF-trained nurses at all times
- Enhanced ability to care for severe cases without transfers to another unit
- Complete digitization of records through the NICU Live digital platform
- On the tip availability of neonatologists ensures advanced guidance and support
- Comprehensive and continuous training program by NICU Live clinicians ensures upskilling of the nursing team in your NICU.

Admissions
- Baby is admitted to the NICU post-delivery from the same hospital or retrieved from a different unit.
- Labs, notes and details are used to admit the patient on the data management portal.

Treatment Plans
- Motherhood tele- intensive care team and hospital team review all patient cases to come up with treatment plans.
- The team executes medical orders.

Patient Management
- 24/7 real-time monitoring.
- Proactive and reactive interventions based on patient severity.
- Guided emergency management.
- Follow up on medications, tests and therapies.

Daily Rounds
- Motherhoodc onducts rounds with hospital team using 2-way A/V.
- In-depth expert review of care plan.
- Multi-disciplinary interaction.

Analytics
- Monthly performance versus benchmarks.
- Clinical quality improvement initiatives.
- Risk mitigation strategies and protocols.

Discharge
- Auto generated discharge summary.
- Discharge care plan shared with specialists and primary physicians.
- Plan transition of care from ICU to ward/home.
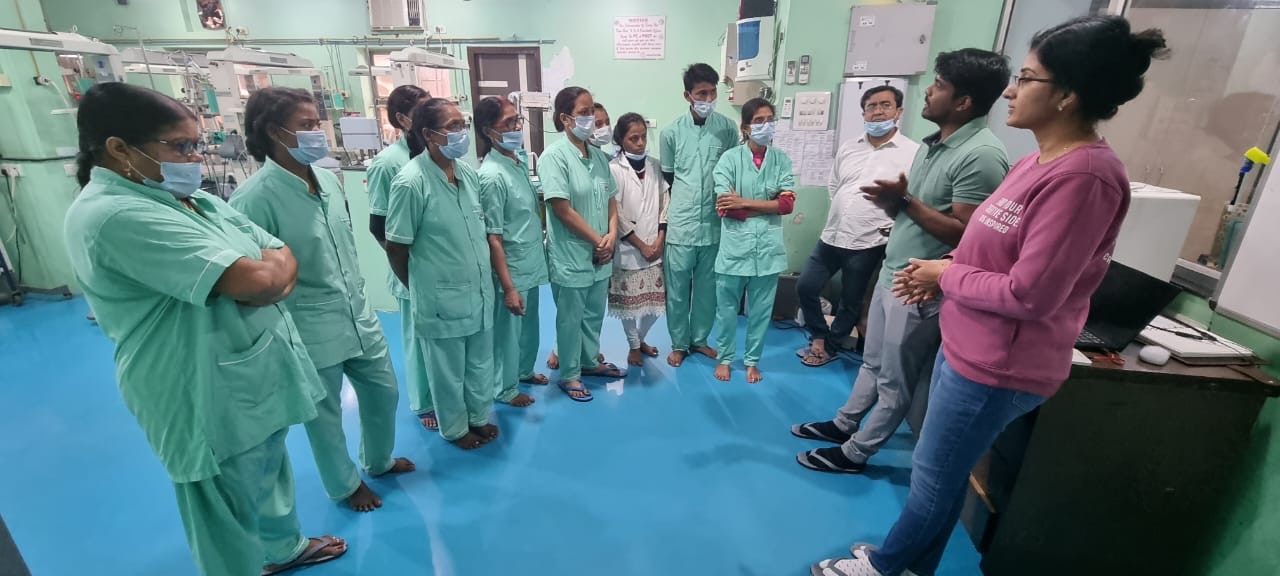
The NICU Live team also provides continuous learning opportunities to the staff at the partner hospital and provides regular training on advance clinical care and implementing best practices









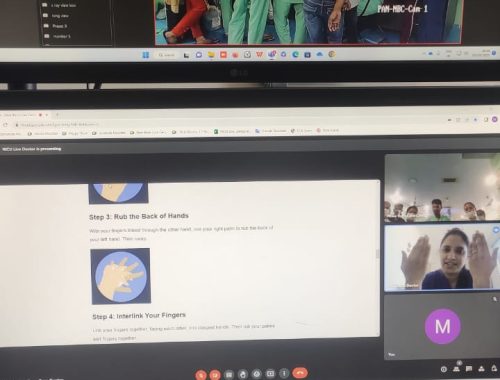
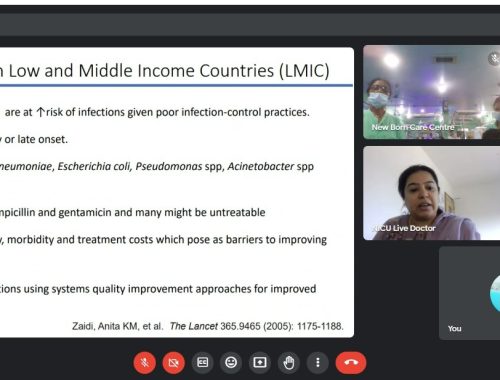
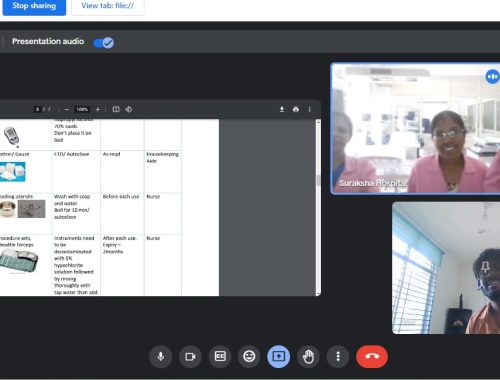
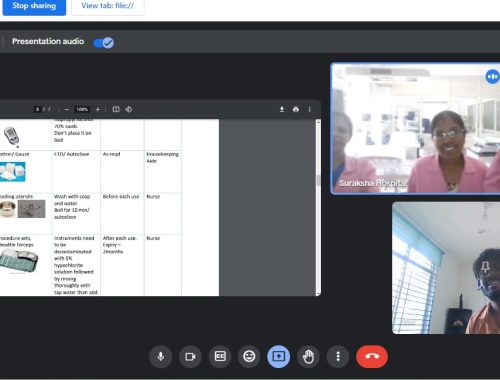



These training modules are designed keeping into consideration the level of the NICU and the current capabilities.
Quality audits and best practice implementation is done with the team to ensure overall quality of the NICU is boosted.
Average 200+ manhours of monthly training is provided by NICU Live
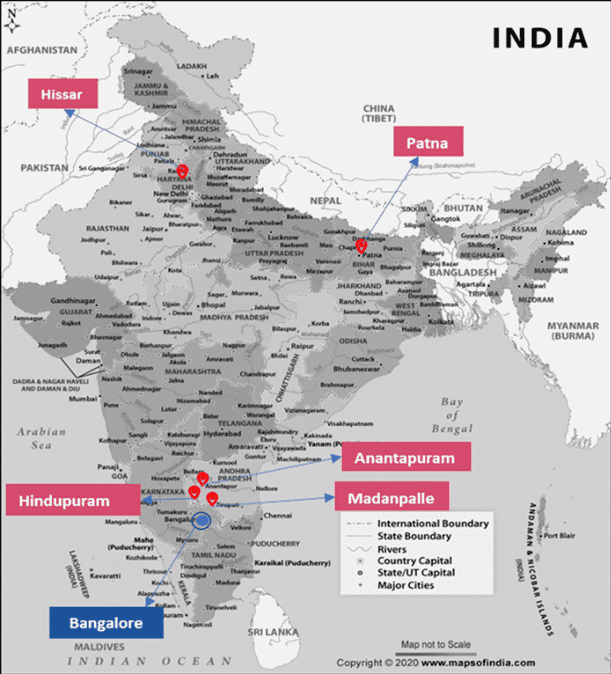
Location
Testimonials
Impact Cases
IMPACT CASE 1:
Neonatal Pleural Effusion

Case Summary:
A newborn baby was admitted to one of NICU Live’s partner hospital with severe difficulty in breathing requiring breathing tube assistance and ventilator care. Surfactant administration and oxygen-enriched air were attempted but did not yield the expected improvement. The newborn was then admitted under the watchful eye of the NICU Live team.
The NICU Live expert team ordered an urgent lung ultrasound to check for fluid surrounding the lungs. USG revealed large effusion around both lungs, for which the doctors were advised to perform pleural tap to remove the excess fluids.
Follow up chest X-Ray showed good lung expansion, showing improvement in the child’s condition. After 48 hours, the child was able to breathe on its own and the breathing tube was removed. There was no fluid accumulation of fluid in any other part of the child’s body. The baby was given antibiotics and nutrition through an IV.
However, 12-hours following initiation of mother’s feeds, the pleural fluid turned milky white and the assessments showed that the effusions had begun again. NICU Live team immediately advised stoppage of Mother’s milk and requested to place the newborn on Octreotide infusion. Under NICU Live doctors’ continuous monitoring and multiple timely interventions, the child stabilized again.
While such cases are relatively rare, without prompt expert medical assistance, it can prove dangerous. The collaboration between the NICU live, expert team and the bed side team helped in identifying correct and timely diagnosis which was further supplemented with the constant support and guidance to the bed side team by the NICU Live experts. This advanced level medical care helped in saving the newborn baby’s life.
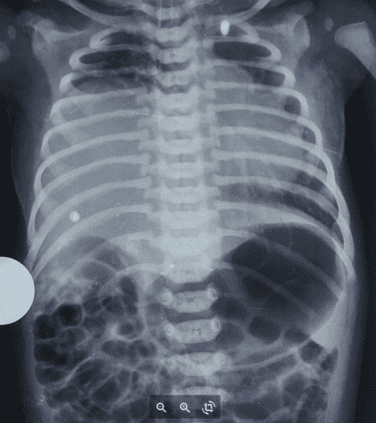
The Case Background
A term baby was admitted with respiratory distress. CXR revealed homogenous whiteout lungs bilaterally. The patient required immediate intubation, which was provided.
After the first dose of surfactant was given, the Fio2 requirement was gradually reduced. The second X-ray showed no changes in the widespread opacity of the lungs. Seeing no improvement, the baby was admitted to NICU Live.
Impact of NICU Live’s Intervention
Urgent lung ultrasound was advised, to evaluate for pleural effusion, and it showed a large effusion. A pleural tap was done, followed by ICD placement. After these procedures, the next X-Ray taken showed well-expanded lungs, with improvement in the condition. The intubation was removed 48 hours later after doctors confirmed there was no accumulation of fluid in any other body spaces. The baby remained on IV antibiotics, and TPN, and was hemodynamically stable.
The assessments through NICU Live continued, and after initial stabilization, doctors recommended that feeds be gradually introduced with caution. However, In the next 12 hours, pleural fluid from ICD turned milky white, indicating chyle. Immediately, the enteral nutrition was stopped. A repeat pleural fluid analysis confirmed chylous effusion bilaterally. The baby was put on Octreotide infusion and it was graded up to achieve a response. After one week of medication, the chyle gradually started reducing. A surgical review was done, and we planned to do chemical pleurodesis if there was no response to octreotide. But the family wanted to take the discharge of the baby, against medical advice.
NICU Live Benefits
While congenital neonatal chylous pleural effusions are relatively rare and require clinical expertise and patience to diagnose and treat, they may turn dangerous if timely medical expert advice is not available. The intervention provided by NICU Live was priceless support to ensure a correct, timely diagnosis of the above case. It enabled the healthcare providers to administer the correct procedures and medication for the recovery of the newborn
IMPACT CASE 2:
Case of the Missing Diaphragm
Case Summary:
A 12-day old baby with difficulty in breathing, on ventilator since birth was admitted to NICU. The baby was managed with a tentative diagnosis of Persistent Pulmonary Hypertension of the Newborn (PPHN). Various efforts by the ground team to get the baby off the ventilator failed. Two days later, the child was admitted to NICU Live.
While being assessed by the NICU team, the baby had an episode of bleeding in the lungs and upper respiratory tract. The baby’s arterial blood gas test showed a PaO2 greater than 150 mm Hg, which is unexpectedly high for PPHN. The administration of surfactant into the lungs resulted in a transient improvement in the baby’s condition.
To investigate the underlying cause of the respiratory distress, an immediate chest ultrasound was performed, revealing a rare condition known as “complete eventration of the diaphragm.” This condition involves the liver being positioned in the right chest cavity, with the diaphragm tissue appearing extremely thin and fibrous.
To investigate the underlying cause of the respiratory distress, an immediate chest ultrasound was performed, revealing a rare condition known as “complete eventration of the diaphragm.” This condition involves the liver being positioned in the right chest cavity, with the diaphragm tissue appearing extremely thin and fibrous.
NICU Live facilitated an immediate multidisciplinary discussion between the NICU team, ground team medical doctors, surgeons, and sonologists. Within four hours of admission to NICU Live, the correct diagnosis was reached, enabling the provision of appropriate and timely care for the baby.
The Case Background
A 12-day-old newborn baby showed respiratory distress, difficult to wean Fio2, requiring 50-70% and above x-ray features. The baby was started on adrenaline and milrinone infusion for mild PPHN features on ECHO. Two days later, the baby was admitted to NICU Live.
NICU Live intervention
During the assessment by the NICU Live team, the baby had an episode of pulmonary hemorrhage. Milrinone infusion was immediately stopped since all ABG until then had PaO2>150. A surfactant dose was given with good recovery.
Given the anatomy of structures on the X-ray taken, there was a strong suspicion of congenital diaphragmatic hernia vs. eventration of the diaphragm.
An immediate chest USG revealed that the liver was in the right chest cavity with a very thin rim of fibrous tissue which did not seem adequate to be a diaphragm. The diagnosis provided by the doctors was a complete diaphragmatic eventration. A surgical consult was taken and the baby was transferred to the surgical center for the probable need for Plication of the diaphragm – due to the eventration.
NICU LIVE Benefits
Congenital complete eventration is a rare occurrence, and almost always, congenital. It requires extremely careful assessment and treatment, especially so in neo-natal cases. Once it is successfully diagnosed, doctors need to work with a high degree of precision to save the infant’s life. It has to be multi-disciplinary coordination – Medical Vs. Surgical. NICU Live was able to communicate between specialties in the
interest of the baby and arrive at a diagnosis that could be effected with proper treatment at the right time.
IMPACT CASE 3:
Thrombosis in Neonates
Case Summary:
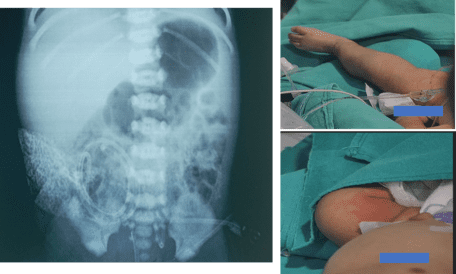
A 40-hour old newborn was admitted to NICU Live with issues of inhaling meconium, (the initial feces formed before birth), along with severe respiratory issues requiring breathing tube and ventilator assistance to survive. Baby was admitted under NICU Live at the partner hospital.
With help of NICU Live, baby was managed using IV antibiotics, IV medications to treat low blood pressures and IV nutrition. IV access is of utmost importance while treating critical babies and the partner hospital was advised that the umbilical venous line be secured, while monitoring the baby. In the next 24 hours, the baby was noticed to have a weak pulse in the left leg, and it had started to go pale/blue in patches and the limp had no activity.
An immediate chest and abdomen X-ray revealed that the venous catheter was wrongly placed in an artery (instead of a vein) supplying the left leg there by completely blocking the blood circulation to left leg. The catheter was immediately removed and blood thinner drip was started. In 6-8 hours, the circulation and muscle tone in the left leg gradually returned.
For newborn patients, it is a common practice to rely on visual cues to differentiate between the umbilical artery and the vein, to place any lines. An improperly placed umbilical line is one of the most common causes for minor and major blood clots in newborns, which causes a shortage of blood supply and oxygen to the limbs. Such shortages can permanently debilitate the infant, and even lead to loss of limb. With timely intervention from the NICU Live team, the left leg was saved thus leading to improvement in the quality of life of the child.
The Case Background
A term neonate was admitted to NICU Live at 40 hours of life with meconium aspiration and severe and Persistent Pulmonary Hypertension. The baby had to be intubated on admission, and blood screened for sepsis. Antibiotics and inotropes were started for the first treatment.
NICU Live intervention
Initial X-ray showed features of meconium aspiration, so the baby was given surfactant, and started on milrinone + noradrenaline via peripheral IV for emergency purposes. Doctors, through NICU Live, advised to secure the umbilical venous line, but in the next 20 hours, the baby showed weak pulses in the left lower limb, with poor perfusion and decreased activity and tone.
Immediate chest and abdomen x-ray was taken to confirm the position of the venous line, and the catheter was found to be malpositioned in the umbilical artery ending at L4-L5 level coinciding with the branching of the common iliac artery. Doppler scan confirmed a thrombus of the left femoral artery. The catheter was removed, the heparin drip started, and circulation was gradually restored in the following 6-8 hours.
NICU LIVE Benefits
For neonatal patients, it is a common practice to rely ONLY on visual caliber differences for identification of umbilical artery and vein to place lines without getting an X-ray to confirm line positions. Malpositioned umbilical lines are the most common cause of neonatal thrombosis and microthrombi, leading to limb ischemia. Therefore, it is prudent to do an x-ray after placing lines to confirm a good position. The timely intervention of NICU Live saved the left lower limb from prolonged ischemia, which might have led to irreversible debilitating consequences affecting the quality of life of the child.

Dr. SREEVIDYA SREEKANTHA
MBBS MD FAAP (Neonatal-Perinatal Medicine)
Recognized for her leadership and expertise, Dr. Sreevidya serves as lead cosultant of NICU Live program. Dr. Sreevidya is a board-certified pediatrician and neonatologist by American Academy of Pediatrics. She completed her medical degree from J.J.M. Medical College, Davangere, India in 2009 and M D Pediatrics from Flushing Hospital Medical Center, New York, USA in 2013. In 2016 she was awarded an M D in Neonatal-Perinatal Medicine from Harbor UCLA Medical Center/Children’s Hospital Orange County (CHOC), California, USA. .
Dr. Sreevidya returned to India in 2019, to serve home country and joined Motherhood Hospitals, Bengaluru as a consultant pediatrician. In 2021, she served as HOD pediatrics at lilfeet, Altius hospital where she set up a robust level III NICU. In October 2022, Dr. Sreevidya joined as Lead consultant NICU Live program at Motherhood India, Bangalore where she is the driving the NICU telemonitoring team.
In 10 years of her experience, Dr. Sreevidya has managed diverse group of medical and surgical conditions like Birth aspyxia, PPHN, Congenital diaphragmatic hernia,cardiac defects, prematurity, sepsis, neonatal ECMO etc.
Her belief of care is to provide family centered care and apply evidence-based practices. She has special interest in perinatology, neonatal hemodynamics and infection control in NICU. She has membership in some of the leading global medical institutions; Karnataka Medical Council 2009, Medical Council of India 2009, and American Medical Association 2013, the American Academy of Pediatrics 2013, and the Medical Board of California 2016, to name a few.
She is also the recipient of the prestigious Pediatric Academic Societies – young investigator award 2019, and the Harbor-UCLA David Imagawa Fellow Award 2019
FAQs
Contact 08069549230 for more details.
For daily NICU operations there is a 24/7 neonatologist- led multidisciplinary team including critical care nurses, dieticians, and pharmacologists that will augment the bedside team. For long-term success, a clinical quality team is assigned to each hospital.
NICU Live engineers can integrate with the hospital’s EMR, LIS, and PAC systems adhering to FHIR/HL7 integration protocols.
NICU Live service includes a strong focus on training and development. Courses offered to include basic life support (BLS) and advanced cardiac life support (ACLS), weekly CNES, and CMEs covering topics like hemodynamic monitoring ventilator management, hand hygiene, antibiotic stewardship, and nutrition training among others.
We give hospitals the confidence to admit more patients and improve NICU utilization. We are flexible to the changing needs of our customers since we are focused on bringing long-term value. We will help the hospital to become a patient’s preferred choice for in-patient care in that community
The mobile app version of the NICU Live management platform is available on both Google and Apple devices. Access patient charts, progress notes, medications, real-time alerts, order entry, and much more. Our game-changing patient-level chat allows medical staff to drop images directly into the patient file.
Reliable internet (leased line or broadband), power back-up, one medical staff per shift who can intubate, and the usual NICU equipment such as x-ray. bedside monitors, crash cart, defibrillator, oxygen supply, ABG, ECG, and IV pumps. If the hospital has NABH/JCI accreditation, we can help maintain operations at those standards
We can onboard a NICU and start managing patients in 2 to 4 weeks
Yes. According to the Telemedicine Practice Guidelines 2020, by the Ministry of Health and Family Welfare, a Registered Medical Practitioner (RMP) is entitled to use telemedicine to consult with another RMP for patients under his/her care. Our solution has role-based access with a 2-step verification process.
NICU Live becomes part of the hospital’s critical care team, working together as one team to deliver high quality care for critically ill patients Our service is full-time and round-the-clock, so the hospital team can rely on our expertise 24/7/365


 Toll Free Number
Toll Free Number