
Endometriosis : The Silent Disease

All You Need To Know About Endometriosis.
Endometriosis-An invisible disease yet painful.The woman suffers and fights within herself.She fights the pain , she fights to explain the unbearable and the unpredictable.Such is the situation of a woman having endometriosis.She has to know as to why she is hurt.She has to know that she has the chance to be pain-free.The below write up will help you to clarify your thoughts regarding endometriosis and to help you to come out of the stigma as well.
What is endometriosis?
The endometrium is the tissue that lines the inside of the womb (uterus).
Endometriosis is a condition where endometrial tissue is found outside the uterus. It is 'trapped' commonly in the pelvic area that is the pelvic cavity (including the ovaries) , lower abdomen and, rarely, in other areas in the body.
Which age group of Women are affected ?
Endometriosis is found almost exclusively in women of reproductive age, with diagnosis done usually during her 30s. It is uncommon in the under-20s.
Endometriosis has a much higher prevalence in infertile women, estimated as between 25% and 40%.
Endometriosis is estimated to affect 10-15% of women of reproductive age.However, it is difficult to determine the prevalence because of the diversity of symptoms and their severity and because endometriosis may be sometimes asymptomatic.
What are the risk factors?
Risk factors include: an early menarche, late menopause, delayed childbearing, short menstrual cycles or long duration of menstrual flow.
Obstruction to vaginal outflow eg, hydrocolpos, female genital mutilation or defects in the uterus or Fallopian tubes.
Genetic factors: Sometimes it runs in families. Therefore, endometriosis is more common in close blood relatives of affected women. Risk for first-degree relatives of women with severe endometriosis is six times higher than that for relatives of unaffected women.
Endometriosis is rare in women past the menopause, as to develop endometriosis you need oestrogen, the female hormone. Oestrogen levels fall after the menopause.
The combined oral contraceptive pill reduces the risk of developing endometriosis. This protective effect may persist for up to a year after stopping 'the pill'.
What are the causes of endometriosis?
There have been several theories over the years.One theory was that some cells from the endometrium gets outside the uterus into the pelvic area. They get there during the monthly periods by spilling backwards along the Fallopian tubes.This is called retrograde menstruation.Other theories are spreading through lymphatic or haematogenous spread, and metaplasia.
However, currently the consensus is that endometriosis has a multifactorial aetiology, involving possible genetic, immunological and endocrinological factors.
What are the symptoms of endometriosis?
The clinical presentation is variable, with some women experiencing several severe symptoms and others having no symptoms at all. The severity of symptoms tends to increase with age.
Women with endometriosis may have no symptoms and be diagnosed incidentally or during investigations for infertility.
The appearance or worsening of pain at the time of menstruation, or just prior to it, suggests endometriosis.
Painful periods The pain typically begins a few days before the period and usually lasts the whole of the period. The pain is different compared to normal period pain which is usually not as severe and doesn't last as long.
Painful intercourse The pain is typically felt deep inside and may last a few hours after intercourse.
Pain in the lower abdomen and pelvic area. Sometimes the pain is constant but it is usually worse on the days just before and during a period.
Other menstrual symptoms may occur - for example, heavy bleeding during periods.
Difficulty becoming pregnant (reduced fertility). This may be due to patches of endometriosis in the ovary which forms cysts and does not allow eggs to grow.
Other symptoms include dysuria that is pain during urination, painful defecation, abdominal pain, backache, menstrual irregularity, and cyclical pain or bleeding (eg, epistaxis, haemoptysis) at extrapelvic sites.
What are the complications of endometriosis?
Infertility: moderate-to-severe endometriosis can cause tubal damage leading to infertility. Lesser degrees of endometriosis, even in the absence of any obvious tubal damage, are also associated with subfertility and increased risk of ectopic pregnancy.
Adhesion formation may occur due to the endometriosis or following surgery.
Women with endometriosis have an increased risk of inflammatory bowel disease.
Endometriosis may also be associated with an increased risk of breast and other cancers, autoimmune and atopic disorders.Rarely it may be associated with invasive ovarian cancer.
What are the other conditions mimicking endometriosis?
- Pelvic inflammatory disease.
- Ectopic pregnancy.
- Torsion of an ovarian cyst.
- Appendicitis.
- Primary dysmenorrhoea.
- Irritable bowel syndrome.
- Uterine fibroids.
- Urinary tract infection.
It??s time to start the conversation It's the conversation of positivity.You need to open up the other side of the conversation.You need to know that you can have better life which is pain free,just by knowing what you need and how to deal with it more better.
How is endometriosis diagnosed and confirmed?
Transvaginal ultrasound scanning appears to be a useful test, both to make and to exclude the diagnosis of an ovarian endometrioma.
MRI scan may be a useful non-invasive tool in diagnosis, especially for subperitoneal deposits.
CA 125 measurement has limited value as a screening test or diagnostic test.
For a definitive diagnosis of most forms of endometriosis, laparoscopy is the gold standard investigation but it is invasive with a small risk of major complications - eg, bowel perforation.On laparoscopic findings, endometriosis is divided into Grade 1 to grade 4.Grade 1 is minimum disease,grade 2 is mild, grade 3 is moderate and Grade 4 endometriosis is severe form.
How is endometriosis treated?
The treatment of endometriosis is usually individually based, depending on the nature and severity of symptoms and the need for future fertility.
Medical treatment may reduce symptoms in 80-90% of patients but none of the treatment options has been shown to reduce recurrence of symptoms once treatment has stopped.
Pain management
The major goal of treatment is to reduce pain.There are 2 options in the management of pain one is non invasive medical line of treatment and the other is invasive surgical line of treatment.
Medical line of treatment
Non-steroidal anti-inflammatory drugsmay be effective in reducing the pain associated with endometriosis, although the evidence to date is inconclusive.Paracetamol, with or without added codeine, is an alternative.
Hormonal drugs: are equally effective: the COCP, danazol, oral or depot medroxyprogesterone acetate are as effective as the GnRH analogues and can be used long-term.Approximately 80-85% of patients improve with treatment.
Ablation of endometrioid lesions reduces endometriosis-associated pain. The smallest effect is seen in patients with minimal disease.
The levonorgestrel intrauterine system has also been shown to be effective.
Surgical line of treatment
Surgical options include removing severe and deeply infiltrating lesions (which may reduce pain related to endometriosis), ovarian cystectomy (for endometriomas), adhesiolysis and bilateral oophorectomy (often with a hysterectomy).Laparoscopic excision or ablation at the time of diagnostic laparoscopy.
The main conservative surgical techniques performed by laparoscopy are thermal or laser ablation, excision, ovarian cystectomy and denervation procedures.
Management of infertility associated with endometriosis
Medical treatment for endometriosis should be avoided for women who are trying to conceive.
In minimal-mild endometriosis, ablation of endometrioid lesions plus adhesiolysis is effective compared to diagnostic laparoscopy alone.
The use of laparoscopic surgery in the treatment of subfertility related to minimal and mild endometriosis may improve future fertility.
In moderate-to-severe endometriosis ,In vitro fertilisation (IVF) is appropriate treatment, especially if there are coexisting causes of infertility and/or other treatments have failed.
Success of treatment and side-effects
Overall, the hormone treatment options, all have about the same success rate at reducing pain.
What is the recurrence rate of endometriosis?
The natural course of the disease is variable and may or may not be progressive
In the five years after surgery or medical treatment, 20-50% of women will have a recurrence. Long-term medical treatment (with or without surgery) has the potential to reduce recurrence but there is no clear evidence for this.
Relapse following surgical treatment is common. 20% recurrence rate at two years and 40-50% at five years is known.
Effect of diet and exercise in endometriosis:
As we know there are a variety of treatments for endometriosis??ranging from medications to surgery??lifestyle changes should not be neglected. We know that lifestyle changes, including what you eat and how much physical activity you get, affect estrogen-dependent conditions like endometriosis.
Unfortunately, there are very few studies on endometriosis and lifestyle focus on whether certain diets or levels of activity are connected to endometriosis.This doesn't mean that they're not worth a try.
Healthy diet and physical activity helps in improved immunity which inturn helps reduce inflammation in endometriosis to some extent.
The following are the lifestyle and dietary changes:
- Following a balanced diet rich in iron, fibre and essential fatty acids (EFAs).
- Increasing physical activity.
- Drinking plenty of water.
- Quitting smoking.
- Avoiding drinking alcohol and caffeine.
Related Blogs

Understanding Gestational Diabetes: Insights from Dr Shruthi Kalagara
Read More
Urinary Tract Infection (UTI) in Pregnancy
Read More
Early Pregnancy Care for New Pregnant Women: Expert Advice | Motherhood Hospitals
Read More
Body Positivity Tips Post C Section (Cesarean Delivery)
Read More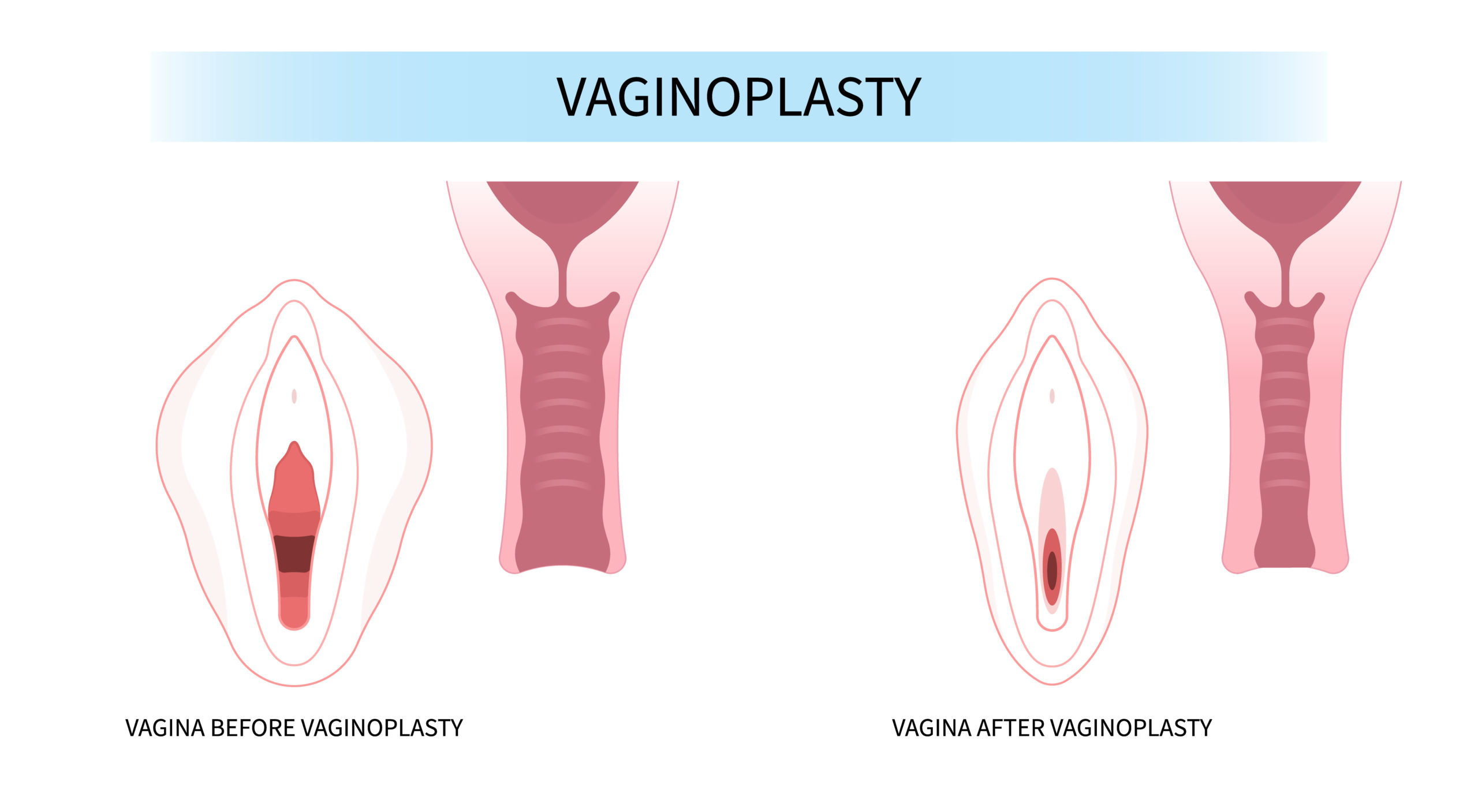
Vaginoplasty: Procedure, Cost, Risks & Benefits, Recovery
Read More
The Digital Dilemma: Exploring the Medical Implications of Technology on Child Development
Read More
How To Relieve Menstrual Cramps? - 8 Simple Tips
Read More
Benefits of Consuming Folic Acid Tablets For Pregnancy/During Pregnancy
Read More
Navigating Radiology: Ensuring Safe Imaging During Pregnancy
Read More
Navigating Radiological Tests During Pregnancy: Ensuring Safety for Mother and Child
Read MoreRequest A Call Back
Leave a Comment:
View Comments
Previous
Next
HELLO,
Stay update don our latest packages, offer, news, new launches, and more. Enter your email to subscribe to our news letter


 Toll Free Number
Toll Free Number








No comment yet, add your voice below!